HORMONAL COIL (IUS)
WHEN and HOW?
When can a Hormonal Coil be inserted?
A hormonal coil (IUS) can be inserted into your uterus at any time of your cycle as long as you are not pregnant.
Please note the following:
- If the hormonal coil is inserted during the first 7 days of your cycle, you are immediately protected from pregnancy.
- If it is inserted at any other time of your cycle, you must use additional contraception, such as condoms, for 7 days.
The hormonal coil (IUS) is highly effective – the efficacy is 99% with typical use.
How is the Hormonal Coil (IUS) placed?
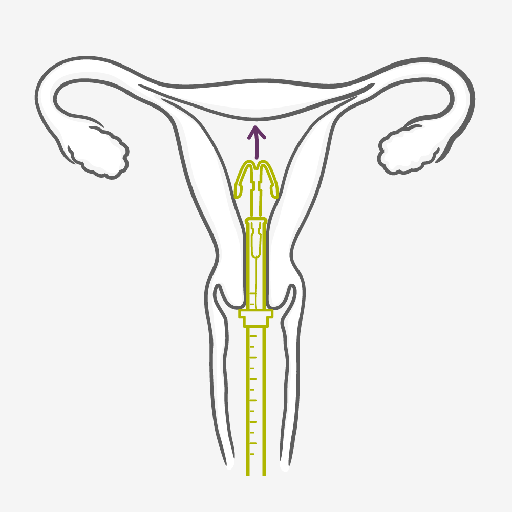
- Before the IUS is inserted, your doctor will check the position and size of your uterus.
- You may also be tested for existing infections, such as STIs, and receive antibiotics.
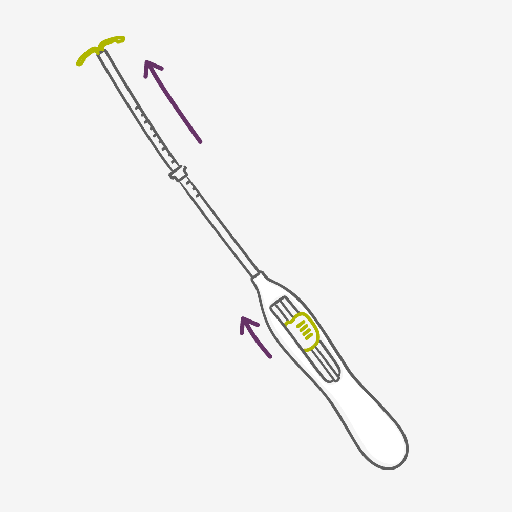
- Your healthcare provider will use an inserter to fit the hormonal coil into your womb. This can be uncomfortable or painful, but you can have a local anesthetic to help. Ask for pain medication (this can be given before or also after the insertion) or local anesthesia.
- If you experience pain or discomfort during the insertion of the hormonal coil, please inform your healthcare provider. You can stop it at any time.
- After the IUS has been inserted, a follow-up appointment is often scheduled to make sure everything is fine. It's important that you keep this appointment.
Once the IUS has been fitted by a well-trained healthcare provider, you’re highly protected from pregnancy from 3 to up to 8 years, depending on the type. Slight period-type cramps may occur afterwards. In case of any concerns please talk to your doctor.
IUS WHEN and HOW?
When can an IUS be inserted?
An IUS can be inserted into your uterus at any time of your cycle as long as you are not pregnant. Please note the following:
- If the IUS is inserted during the first 7 days of your cycle, you are immediately protected from pregnancy.
- If it is inserted at any other time of your cycle, you must use additional contraception, such as condoms, for 7 days.
How is the IUS placed?
- Before the IUS is inserted, your doctor will check the position and size of your uterus.
- You may also be tested for existing infections, such as STIs, and receive antibiotics.
- Your healthcare provider will use an inserter to fit the IUS into your womb.
This can be uncomfortable or painful, but you can have a local anesthetic to help. Please discuss this with your doctor in advance.
- Ask for pain medication (this can be given before or also after the insertion) or local anesthesia.
- If you experience pain or discomfort during the insertion of the IUS, please inform your healthcare provider. You can stop it at any time.
- After the IUS has been inserted, a follow-up appointment is often scheduled to make sure everything is fine. It's important that you keep this appointment.
Once the IUS has been fitted by a well-trained healthcare provider, you’re highly protected from pregnancy for up to 3 or 5 years, depending on the type.
Slight period-type cramps may occur afterwards. In case of any concerns please talk to your doctor.
Tabs header
HORMONAL COIL (IUS) PROS:
- It can stay in place for either 3 or 8 years (depending on the type), but can be removed any time.
- At 99.8%, it’s one of the most effective contraceptive methods
- It doesn’t interrupt sex
- Heavy periods can become lighter and less painful
- Some women may have shorter lighter or less frequent periods, which reduces the chances of becoming anemic
- Suitable for women who want long-acting reversible contraception for up to 3 or 8 years and wish to avoid daily, weekly or monthly regimens
- It can be used when breastfeeding
- Fertility returns to its previous level once the hormonal coil (IUS) is removed
HORMONAL COIL (IUS) CONS:
- It requires a trained healthcare provider for insertion and removal
- Irregular bleeding and spotting can be common in the first 6 months of use
- Some women experience headaches, tenderness and acne after an IUS is fitted
- It may cause cramps and/or irregular bleeding
- Small risk of infection at insertion and of expulsion
- Does not protect against HIV infection (AIDS) and other sexually transmitted infections (STIs)
- It is rare but the IUS can come through the wall of the womb when it is put in (fewer than 2 in 1000)
- Pregnancy outside the womb (ectopic pregnancy) is possible but very rare.
All important details about the Hormonal Coil (IUS)
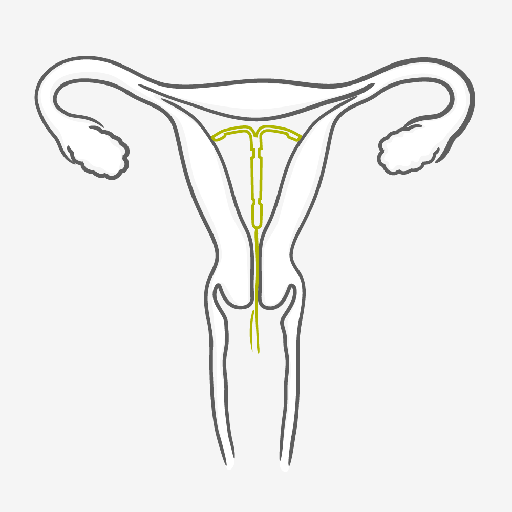
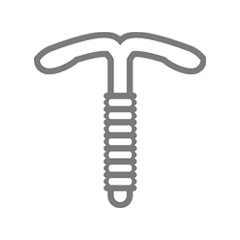
The hormonal coil also called IUS (Intrauterine System) is a small, soft, T-shaped device with a reservoir containing the hormone progestin that is placed in the womb by your healthcare provider. The IUS works by continuously releasing a low dose of progestin from the intrauterine system into the womb. It thickens the mucus of your cervix, which makes it harder for sperm to move freely and reach the egg and it also thins the lining of your uterus. At 99.8% efficacy, you’re about as protected as you possibly can be by a contraceptive method. You’re highly protected from pregnancy from 3 to up to 8 years, depending on the type. It’s a great method for the super organized, the forgetful, the frequent traveler and pretty much anyone else who is keen on staying not pregnant. However, there are some individual risk factors that make hormonal coils not recommendable to some women. Therefore, consult your healthcare provider to find out about your individual situation.

Questions & Answers about the Hormonal Coil
FREQUENTLY ASKED QUESTIONS
The insertion is usually well tolerated by most women. Some women may experience pain and dizziness after insertion, which usually settles after resting for a short time. Normal pain killers or local anesthesia may be applied to the uterine cervix prior to the insertion.
The IUS has not been approved for use as emergency contraception. Please ask your doctor for further advice.
The hormonal coil must be inserted by a trained healthcare provider, who will follow the necessary procedure to ensure it is correctly positioned. Occasionally, the muscular contractions of the womb during menstruation may sometimes push it out of place or expel it. Very rarely it can perforate the wall of the uterus. If a user of an IUS experiences any unusual bleeding, pain or discomfort, the doctor or healthcare provider must be informed as soon as possible.
Neither you nor your partner should feel the hormonal coil during sexual intercourse. If you do, sexual intercourse should be avoided until your doctor or healthcare provider has checked that the hormonal coil is still in the correct position.
The copper coil (IUD) is a small plastic T-shaped device covered by copper or other metals which is inserted in the cavity of the womb. The hormonal coil (IUS) is made of two components: the plastic T-shaped device and a cylinder containing progestin hormone, which is released slowly from the system. Both coils have a number of different characteristics and work in a different way. Talk to your doctor or healthcare provider to find out which option is more appropriate for you.
Use of sanitary pads is recommended. If tampons are used, you should change them more frequently the first month after the coil insertion.
The progestin released from the hormonal coil causes the lining of the uterus to become very thin. Therefore it can change your menstrual periods so that you can have shorter or longer periods, lighter or heavier bleeding, or no bleeding at all. When the hormonal coil is first inserted, before the lining becomes completely thinned out, women may have unpredictable spotting (a small amount of blood loss). This usually clears after the first months following insertion. If it does not clear, then you should see your doctor or healthcare provider to make sure there is not another cause for the bleeding.
Many women with a hormonal coil will experience less and lighter bleeding after the coil is fitted. Some women may not have any periods at all anymore.
The hormonal coil can be left in place for up to three or eight years depending in the type. After this time, it will need to be replaced with a new device. If this method of contraception has worked well for you, and if you still wish to use a long-term contraceptive option, then you can discuss with your healthcare provider about continuing with this method.